Presentation of a Case
A 20-year-old white woman came in with fever, chills, widespread joint pain, photosensitivity, tiredness, and myalgia that had been going on for four weeks. In the past three days, she had been stiff in the morning for more than an hour and had been getting short of breath over time. She also said she had been getting mouth ulcers over and over again for the past month that didn’t hurt. Besides that, she didn’t have any stomach problems like pain, blood, sickness, vomiting, or changes in her bowel habits. There was no history of losing weight, having night sweats, getting certain skin spots, or having Raynaud’s phenomenon signs in the limbs. The patient said they had never used drugs, alcohol, or tobacco, and they had no medical background. As a housewife, she hadn’t recently been around anyone with similar symptoms, and her family background and travels in the last six months were also clean. The person had all of their necessary vaccines up to date.
The patient had been in the hospital for three days two weeks before this stay. During that time, she had a fever of unknown cause (FUO), which was treated with metronidazole and cefixime. Even so, her symptoms didn’t get better and got worse over time, which is what led to her present stay.
Looking at
The patient’s body temperature was 39 °C, their heart rate was 75 beats per minute, they breathed 15 times per minute, their blood pressure was 110/75 mmHg, and their oxygen saturation was 97% when they were breathing normal air. She looked very sick and weak, but she was awake, aware, and able to answer questions. On physical exam, there were 2 cm in diameter of rubbery, soft, and movable lymph nodes on the right side of the neck and supraclavicular area. There were no signs of disease. When the abdomen was touched, there were no signs of hepatomegaly or splenomegaly. An mouth exam showed a single 2 cm tumor in the buccal mucosa that was covered in fluids and had a red border around it. There were no signs of blisters. A look at the skin didn’t reveal any common skin problems like a malar rash. There was also no sign of recent severe inflammation in the joints or a vaginal aphthous sore.
Look into it
After a full blood count (CBC), the white blood cell count was 3.1 × 109/L, the hemoglobin number was 9 g/dL, and the platelet count was 320 × 109/L. The amounts of aspartate aminotransferase (AST), alanine aminotransferase (ALT), and alkaline phosphatase (ALP) in the blood were all normal. The lab test results showed that the erythrocyte sedimentation rate (ESR) was 74 mm/hour, the C-reactive protein (CRP) was 69 mg/L, and the lactate dehydrogenase (LDH) level was 1324 IU/L (normal values are 140–280 IU/L). Crops of blood and pee did not grow any microbes.
Using the HITACHI Roche Cobas C311 chemistry analyzer and enzyme-linked immunosorbent assay (ELISA), tests for Coombs Wright, 2-mercaptoethanol (2ME), perinuclear anti-neutrophil cytoplasmic antibody (p-ANCA), and cytoplasmic anti-neutrophil cytoplasmic antibody (c-ANCA) all came back negative. The person did not have HIV, liver viruses, Epstein-Barr virus (EBV), or cytomegalovirus (CMV). Both the Venereal Disease Research Laboratory (VDRL) and the Fluorescent Treponemal Antibody Absorption (FTA-ABS) tests came back negative. The mouth sore did not have the herpes simplex virus (HSV) on a Tzanck test. There were amounts of antinuclear antibody (ANA) and double-strand DNA antibody (dsDNA) that were positive, as well as small amounts of C3 and C4 complements. The person was told they had systemic lupus erythematosus (SLE) based on standards set by the Systemic Lupus International Collaborating Clinics.
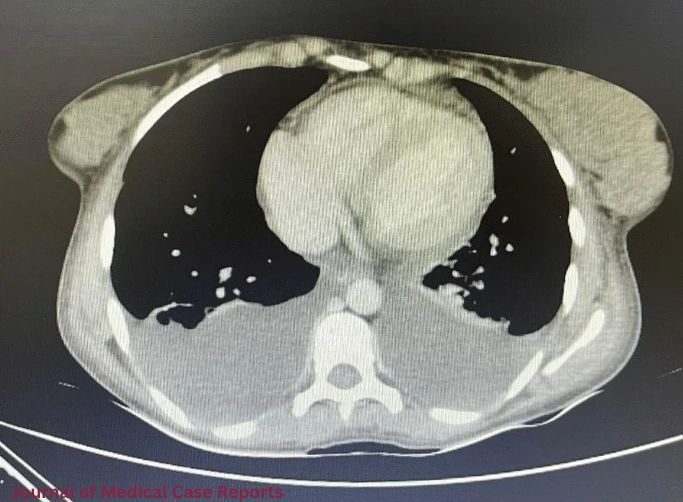
A chest x-ray (CXR) and chest computed tomography (CT) scan showed that both lungs had pleural fluid, which is why both chest tubes were put in. The fluid in the pleura was transudate. A heart ultrasound showed a slight pericardial fluid without endocardial growth.
More tests were done by doctors to figure out how bad the lymphadenopathy was. An ultrasound of the neck showed swollen lymph nodes under the jaw and above the collarbone. The biggest one was 2.5 cm across. A CT scan of the abdomen and pelvis did not show any lymphadenopathy, but it did show hypodense areas in the seventh and sixth segments of the liver.
To find out more, a lymph node biopsy was done with the help of an ultrasound. The results showed that the structure was still there, but there was follicular hypertrophy and necrotizing lymphadenitis with paracortical coagulative necrosis. Immunohistochemistry showed that CD68 and CD4 were expressed, which is consistent with Kikuchi-Fujimoto disease (KFD). A liver core sample from a low-density area also showed limited lobular hepatocyte death and inflammation with histiocytic neutrophils.
Systemic Lupus Erythematosus: How to Treat It
After that, the patient was told that they had KFD-associated systemic lupus erythematosus (SLE) with liver involvement that was not limited to the nodes. Hydroxychloroquine (HCQ) and oral corticosteroids (prednisolone) were used to treat the disease. The patient’s situation improved after five days in the hospital, and she was sent home in good health. After two months of treatment, the lymphadenopathies got better and better until they were gone for good. After six months of regular checks, the symptoms did not come back.
People who have Kikuchi-Fujimoto disease and Systemic Lupus Erythematosus
Kikuchi-Fujimoto disease (KFD), which is also known as histiocytic necrotizing lymphadenitis, is a rare systemic disease that mostly affects young Asian women, though cases have been reported all over the world. KFD can happen to anyone at any age, but most of the time it happens to people under 40.
KFD usually shows up as painful, swollen, and mild necrotizing lymphadenopathy, often with a low-grade fever and tiredness. Headaches, nausea, puking, feeling sick, losing weight, arthralgia, myalgia, night sweats, rashes, and pain in the thorax or abdomen are some of the other symptoms that may happen. KFD can also happen in places other than the nodes, like the skin, bone marrow, and liver, though this is not common. A histological study of lymph nodes usually shows a structure that is only partly intact, with areas of follicular growth and clear areas of necrosis. Different people have different lab readings. Some have average numbers, while others may have anemia, high ESR, CRP, blood LDH, aminotransferases, or leukopenia.
KFD can be mistaken for other infectious, autoimmune, or cancerous diseases because its signs are not always clear. Even though the disease goes away on its own, it is important to get a quick and correct evaluation so that severe treatments are not needed. This study shows a unique case of KFD that affected the liver at the same time as systemic lupus erythematosus (SLE).